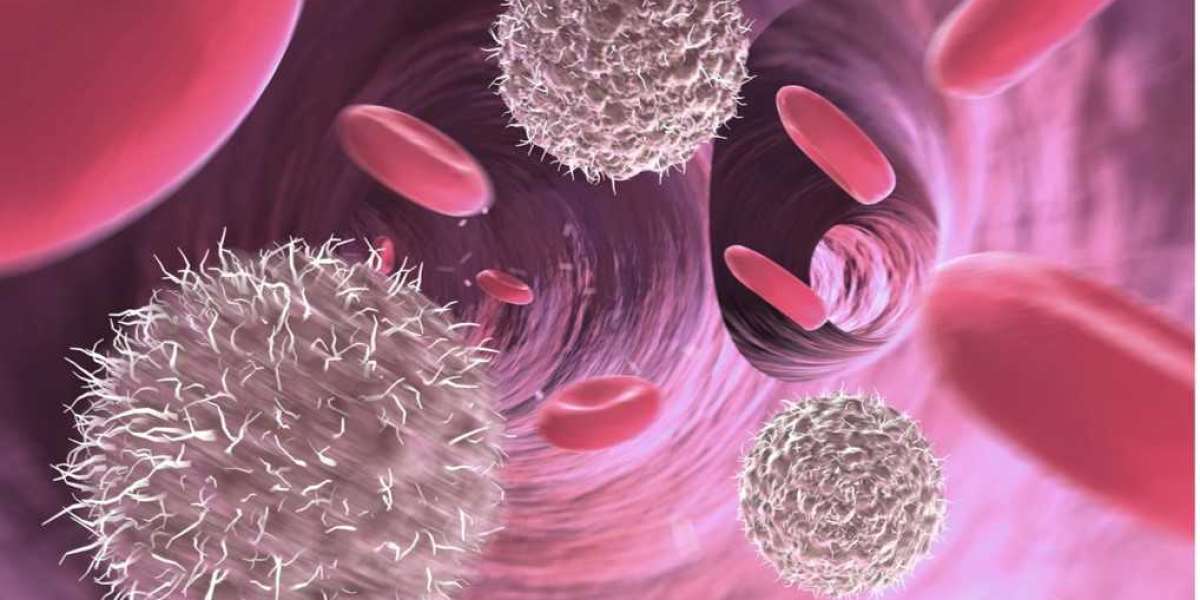
DLBCL is the most common type of non-Hodgkin lymphoma, in which lymphocytes increase in large B-cells with no explanation in the lymphatic system. About two-thirds of the DLBCL cases are treatable with the regular regimens, like R-CHOP (rituximab plus chemotherapy), but, still, there are some patients who relapse after they received a therapy which had seemed to work for them at first, or who are non-responsive to treatment altogether.
There have been challenges associated with cured or resistant (r/r) DLBCL treatment; this is especially so given it is the area which at present lacks maximum management. Nevertheless, a wide spectrum of recently available therapies are now in place that can dramatically change the fate of battling with TB patients.
Novel Antibodies
Since decades rituximab is a proven therapeutic monoclonal antibody to fight with DLBCL, new antibodies that work on different molecular entities are emerging in strong usage in the treatment of relapsed/refractory diseases. The Polatuzumab vedotin-piiq antibody drug conjugate is an agent that binds CD79b, a protein commonly stained by DLBCL cells. In 2019, for the first time an updated drug bending bent specifically to interaction with targeted DLBCL was approved by the FDA in over 30 years.
Followed by a randomized Phase 3 trial comparing polatuzumab vedotin in combination with bendamustine and obinutuzumab to bendamustine plus rituximab, the safety and efficacy of the drug when used for relapsed/refractory DLBCL patients were shown to be significantly higher complete response rates. In 2019, the FDA approved this triplet treatment for the patients in question, after the study results demonstrated its potential.
In addition to other potential therapies in the pipeline, such as tafasitamab-cxix and loncastuximab tesirine that achieved accelerated FDA approval in the last year, have also displayed remarkable results in relapsed/refractory DLBCL. With Tafasitamab the CD19 protein that is found on B cells is targeted and the other type is the loncastuximab tesirine which like its namesake is another antibody-drug conjugate that binds to CD19 and in its turn releases in cancer cells a powerful cytotoxic drug. They both constitute in-novation beyond the usual treatment methods that are being used in the health sector now.
CAR T-Cell Therapy
As antibody drugs can help in the hyper-targeted transport of the pathogen into the lymphoma cell to destroy it, CAR T-cell therapeutics represent another level of personalized therapy, in which a patient's own cells are re-programmed to become a defensive tool. This constitutes a new version of immunotherapy, the first step of which is the patient's own T cells isolation, and the second one is the gene engineering of these T cells to express special proteins called chimeric antigen receptors (CARs) on their surface. In the lab, the CAR T-cells are genetically modified and massively multiplied to later be re-administered into the patient's body and, therefore, become more specific to target and kill the lymphoma cells.
The first two the CAR T cell therapies axicabtagene ciloleucel (Yescarta) and tisagenlecleucel (Kymriah) were approved for emtance therapy in the larger of DLBCL after a big phase of the clinical trials which demonstrated the positive rate of response. ZUMA-1, a phase 2 trial, enrolled r/r DLBCL patients who received axicabtagene ciloleucel where 82% of the participants responded well to the treatment with 58% of the patients responding with the complete repair. Just the same, single-agent tisagenlecleucel urging on 54% of patients in the JULIET study overall.
CAR T-cell therapy is a complex targeted therapy; at the same time it is a personalized and sometimes complex treatment that can bear significant side effects like cytokine release syndrome and neurotoxicity. Still, it has proven to be a good alternative for patients who have exhausted other types of therapy. Will addition of other CAR T-cell products that target different antigens and use new approaches to improve efficacy and safety become the topics for research is also not clear.
Bispecific Antibodies
As the most promising and clinically and technologically sophisticated new generation of medicines, the double specific antibodies (babs) that bind two different biological targets comprise a single molecule are introduced.
These molecules operate through the joint binding of a protein on cancer cells and also one on immune cells. One of the approaches is T cells and natural killer (NK) cells are directly recruited by the immune cells’ killing power against tumors.
Improved efficacy of monoclonal antibody mosunetuzumab which is more harmful to the disease of r/r DLBCL, was confirmed during the clinical trial. It binds to two antigen: CD20 protein on B cells and CD3, further recruits T cells to by specific recognition and destruction of malignant cells that are CD20 positive. As monotherapy mosunetuzumab made complete responses in 37% of r/r DLBCL patients that manifested only the milder toxicity in most cases.
Apart from these CD20 bispecific antibodies, more studies are ongoing to identify CD3, CD19, and CD22 antigens which other bispecific antibodies might also target. Being more effective than single immunotherapeutic treatments in clinical development, some of them have exciting early efficacy signals. Unlike tailored CAR T-cell treatment, these substances come from the humanized anti-cancer molecules that offer personalized immunotherapy which is shorter in duration of treatment.
Despite the grim prognosis of previously treated LBCL having notoriously been poor, these newly developed antibody and immunotherapy drugs are already leading to the revamping of the scheme of treatment for these cases. The best cancer hospital in Hyderabad opines that the purpose of research is the apparent union of novel therapies formulated so as to definitely increase the remission period as well as the overall prognosis in this tumor.
But, it is important to emphasize that proper selection of treatment by patient fitness, medical history and comorbidity are the key factors for success of every method of cardiac rehabilitation. While in the previous context catastrophic outcomes were possible, the current moment has drastically changed bringing a variety of options to the table of the patients that are able to induce long-term responses - something which would be considered unbelievable just a few years ago. Further innovation such as bispecific antibodies drug conjugate and chemotherapy regimen can be anticancer killers. This great future never seems far from the present.
With continued research on the characterization of genomic alterations, dissemination of genetic information, and availability of patient navigation strategies, we anticipate a roadmap for personalized medicine in DLBCL that will ultimately benefit patients, doctors, and researchers alike. As CAR-T cell immunotherapy or precision antibodies agents that have been designed specifically for this cancer become available, clinical teams have far more weapons than earlier for cancer fighting.
Of course, we should not stop here: more research will be needed in the future to optimize positive effects of novel therapies and eliminate the possibility of severe side effects that are inherent for some of these new methods. The best cancer hospital in Bangalore opines that Identification of biomarkers for selection of preferred therapy, developing combination treatments rationally and learning what the cells are doing to resist drugs will be the three major areas to unveil going forward.
Certainly, despite the current difficulties, the fact that in the last few years we have made progress, may give some hope that we are getting better at dealing with these problems. This phase of many exciting innovative therapies, which started earlier as results of encouraging clinical trials, gets a vital inflection point as it transforms from one of theoretical promises to FDA-approved reality.
The patient is relieved to learn that relapsed/refractory DLBCL is no longer seen as a direct line for an easy death sentence. The good news that the disease setting which less than two years ago was a tough therapeutically can now be the reason for optimism that the treatment response can persist durably and probably lead to the cure.
Beside oncologists and patients, each new technological breakthrough is a new chance to save a life by providing another weapon to fight this treated cancer. Periods of remission of diffuse large B-cell lymphoma will soon thrive with the glowing shades of development and desire.
Novel treatments like antibody drugs, CAR T-cell therapy, and bispecific antibodies are transforming outcomes for relapsed/refractory diffuse large B-cell lymphoma. These FDA-approved therapies provide new hope after standard treatments fail in this aggressive blood cancer.